There has been a lot of hype and noise surrounding Steve Jobs' appearance at the WWDC conference and not just because of the new iPhone launch either. His gaunt appearance started a furore amongst the tech analysts and journalists as to how his health was, it was material they claimed.
Thus the setting was established for a interesting battle over someone's privacy and control versus the media herd wanting 'honesty'. Yet, Jobs has been very honest up front - his surgery for early stage pancreatic cancer is well known, no more need be said it's a private matter after that. Image by Getty Images via Daylife
Image by Getty Images via Daylife
The same journalists who praise research and information about stocks should practice what they preach and check out pancreatic cancer, it's all in the public domain. Fifteen minutes spent researching and reading about the topic would tell them all they need to know, without the rather distasteful and rather slimey hounding that is going on at present. Perhaps it's laziness, but sometimes I'm surprised that people who claim to be experts in one area cannot be bothered to research another in the public domain. It makes you wonder what their motives are, especially in the middle of a new product launch for the 3G iPhone.
Take another recent example, Prof Randy Pausch, who sadly died this week from pancreatic cancer. Late last year he gave an inspirational lecture at Carnegie Mellon University but made it clear up front what he wanted to talk about and what was off limits, ie his cancer and his family. His boundaries, like Jobs, on privacy were clear just as the initial medical condition was in both situations. After that, it's nobody's business, you can make your own judgements and act accordingly.
This issue is not about control or honesty, it's about money and greed for the investors. A little bit of research goes a long way, even the analysts will tell a novice investor that, so it cuts both ways.
We also have to remember that the media prey on negative news and 'noise' to generate interest and readership. You don't see much cheerful or good news do you? It's negative and fearful. Good news doesn't sell. Sadly.
Monday, July 28, 2008
Cancer: the privacy vs. honesty argument
Friday, July 25, 2008
Ethnicity and breast cancer - does it matter?
Breast cancer research needs to evaluate whether a person's ethnicity influences their response to treatment and its outcome, according to researchers at Imperial College London and published in The Lancet online.
Emerging evidence suggests that particular drugs may benefit people from one ethnic group more than others, because of differences in their genetic makeup. Most key trials looking at treatments for breast cancer have been carried out in predominantly caucasian populations in Europe, North America and Australasia.
Other populations might not respond to a drug in the same way as the Caucasian populations in these trials. The researchers suggested that clinical trials should record participants' ethnicity and analyse whether there are differences in how patients from particular ethnic groups respond to a particular therapy.
One example is a drug called Herceptin (trastuzumab), which is commonly used to treat people with breast cancer that is HER-2 positive. Most studies of trastuzumab have not reported the ethnicity of participants. A recent study showed that people with a particular genotype responded better than others to treatment with this drug. The genotype in question is more common in some ethnic groups than in others, so it could be argued that an individual's ethnicity could be a key factor in determining which treatments are most likely to benefit them.
Another research group at the University of Miami, Fl has been looking at whether breast tissue samples from different ethnicities include groups of differentially expressed genes. Gene expression in breast tissue from African-American women differs
from that in Caucasian and Hispanic women, just as gene expression in Hispanic women differs from both African-American and Caucasian women.
In their latest study, Baumbach et al. are focusing on women with “triple-negative” breast cancer. These women are negative for the genes for estrogen receptor (ER), progesterone receptor (PR) and HER2/neu, an epidermal growth factor receptor. This combination is associated with a particularly poor prognosis.
Thee results showed surprising differences in normal tissues; some of the differences were specific to African-Americans and were not found in Hispanics or Caucasians. They tended to have a basal-like phenotype and to have an aggressive form of breast cancer before the age of 50. The research also showed that in considering BRCA1 and BRCA2, while they had a lower incidence of deleterious germline mutations but a higher number of missense mutations. They are now doing real time PCR analyses to see if the biggest differences can be validated and proteomic research will follow in the future, making this a large and very important long term study that may influence treatment paradigms in the future.
Sunday, July 20, 2008
Does diet affect your risk of developing prostate cancer?
It is scientific fact that Japan has a lower incidence of prostate cancer unless the Japanese men move to western societies and eat a different diet.
This short but compelling video explains what factors may increase the risk of developing prostate cancer:
Video
Are you as informed as you should be?
Monday, July 14, 2008
Promising new tool for monitoring lung cancer
A non-surgical technique that may help doctors monitor how well non-small cell lung cancer patients are responding to treatment is currently being tested. Using a device known as a CTC-chip to analyze circulating tumour cells from patient's blood samples, it was possible to identify whether patients had genetic mutations that would make them less likely to respond to certain therapies.
The research, published in the New England Journal of Medicine, is still in the early stages. However, if future studies confirm it works, the technique could offer lung cancer patients a non-invasive, safe way to monitor their disease and find out which treatments will work. Currently, in order to get that type of information, patients would have to undergo dangerous, invasive procedures to sample tissues and cells.
The current findings will need to be replicated in larger studies before the chip is used widely, since only 27 patients participated in the pilot study.
The CTC-chip opens up a whole new field of studying tumors in real time. When the device is ready for larger clinical trials, it should provide new ways of measuring treatment response, defining prognostic and predictive measures, and studying the biology of blood-borne metastasis, which is the primary method by which cancer spreads and becomes lethal.
Blood samples from 27 patients, 23 of whom had a cell-surface protein mutation known as the epidermal growth factor receptor (EGFR) mutation were tested. Using the CTC-chip, the researchers were able to identify the mutation from the circulating blood tumour cells 92% of the time.
It was also noticed the chip could detect changes over time. Research has shown that tumours with the EGFR mutation are more likely to respond to a class of drugs known as tyrosine kinase inhibitors, or TKIs; Tarceva (erlotinib) and Iressa (gefitinib) are 2 TKIs used to treat lung cancer. However, the patient's tumours eventually come back. Using the CTC-chip, the researchers found out why; it appears that the tumour cell's genetic makeup evolved over the course of treatment.
Biopsy samples taken at the time of diagnosis can never tell us about changes emerging during therapy or genotypic differences that may occur in different sites of the original tumour, but the CTC-chip offers the promise of noninvasive continuous monitoring.
This information could one day help doctors see when a patient was becoming resistant to treatment so that new therapies could be tried earlier. However, there is still work to do to make this technique more efficient on the larger scale outside of the clinical trial setting.
Monday, July 7, 2008
More on the cancer vaccine front
Hot off the press with the negative news surrounding Gardasil and its paralysis side effects, comes the news that another cancer vaccine, Oncophage (Antigenics), failed to demonstrate sufficient efficacy in renal cell cancer in a phase III trial.
The data was published in The Lancet online.
The accompanying editorial, from James Yang, a respected physician from the NCI, criticised the company for its over enthusiastic and misleading press releases, noting that:
"The credibility of the field of cancer immunotherapy is weakened when some investigators, and particularly vaccine companies, cannot accept the results of randomized trials."
Wednesday, July 2, 2008
Will infusing granulocytes cure human cancer?
Scientists at Wake Forest University Baptist Medical Center are about to begin a trial to determine whether a new cancer treatment will be as effective at eradicating cancer in humans as it has proven to be in mice.
The treatment will involve transfusing specific white blood cells, called granulocytes into patients with advanced forms of cancer. A similar treatment using white blood cells from cancer-resistant mice has previously been highly successful, curing 100 percent of lab mice afflicted with advanced malignancies.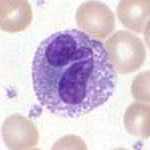 Granulocyte - image via WikipediaThe study is being announced on June 28 at the Understanding Aging conference in Los Angeles. It will involve treating cancer patients with white blood cells from healthy young people whose immune systems produce cells with high levels of cancer-fighting activity.
Granulocyte - image via WikipediaThe study is being announced on June 28 at the Understanding Aging conference in Los Angeles. It will involve treating cancer patients with white blood cells from healthy young people whose immune systems produce cells with high levels of cancer-fighting activity.
The basis of the study was the discovery of a cancer-resistant mouse and their subsequent finding that white blood cells from that mouse and its offspring cured advanced cancers in ordinary laboratory mice. They have since identified similar cancer-killing activity in the white blood cells of some healthy humans.
Human cancer-fighting cells from healthy donors have been tested against human cervical, prostate and breast cancer cells in the laboratory, with good results. The scientists say the anti-tumor response primarily involves granulocytes of the innate immune system, a system known for fighting off infections.
Granulocytes are the most abundant type of white blood cells and can account for as much as 60 percent of total circulating white blood cells in healthy humans. Donors can give granulocytes specifically without losing other components of blood through a process called apheresis that separates granulocytes and returns other blood components back to donors.
In a small study of human volunteers, it was found that cancer-killing activity in the granulocytes was highest in people under age 50. This activity can be lowered by factors such as winter or emotional stress. They said the key to the success for the new therapy is to transfuse sufficient granulocytes from healthy donors while their cancer-killing activities are at their peak level.
For the upcoming study, 500 local potential donors who are 50 years old or younger and in good health are being recruited to have their blood tested. Of those, 100 volunteers with high cancer-killing activity will be asked to donate white blood cells for the study. Cell recipients will include 22 cancer patients who have solid tumours that either didn't respond originally, or no longer respond, to conventional therapies.
The goal of the phase II study is to determine whether patients can tolerate a sufficient amount of transfused granulocytes for the treatment. Participants will be monitored on a regular basis, and after three months scientists will evaluate whether the treatment results in clear clinical benefits for the patients. If this phase of the study is successful, the study will be expanded to determine if the treatment is best suited to certain types of cancer.
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=85e2ca54-518a-41e9-b848-2b1bbd12bc0d)



